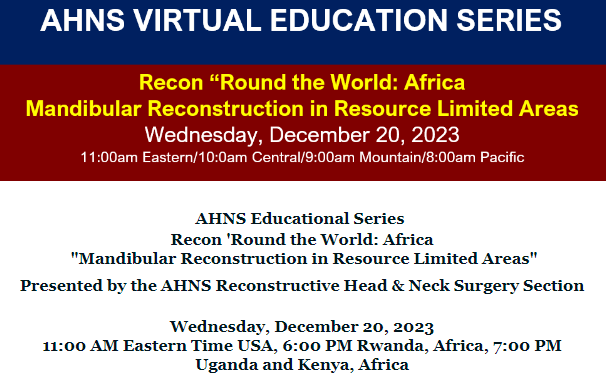
AHNS Educational Series – Recon ‘Round the World: Africa “Mandibular Reconstruction in Resource Limited Areas”
Moderator: Dr. Chad Zender Panelists: Dr. Sarah Rohde Dr. Joyce Aswani Dr. Jeff Otiti Dr. Amol Kulkani Dr. Nathaniel Peterson Session description: This webinar highlights important considerations when treating mandibular tumors of the head and neck in resource limited environments. A panel of clinicians from throughout the continent lend their expertise on this topic. This …