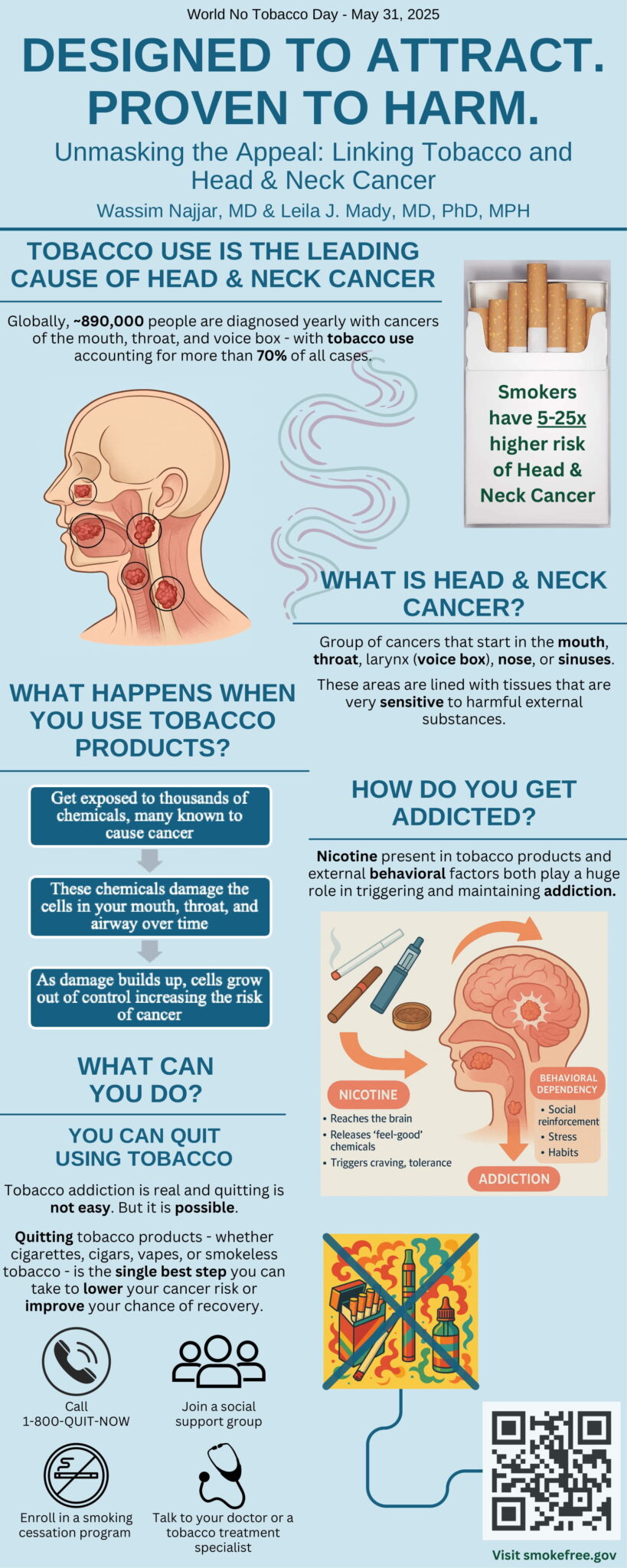
World No Tobacco Day
Tobacco is the leading cause of head and neck cancers — but you can lower your risk. This World No Tobacco Day, we’re raising awareness about how tobacco use increases the risk of cancers in the mouth, throat, and voice box. What can you do? Quitting tobacco today can lower your risk and make a …