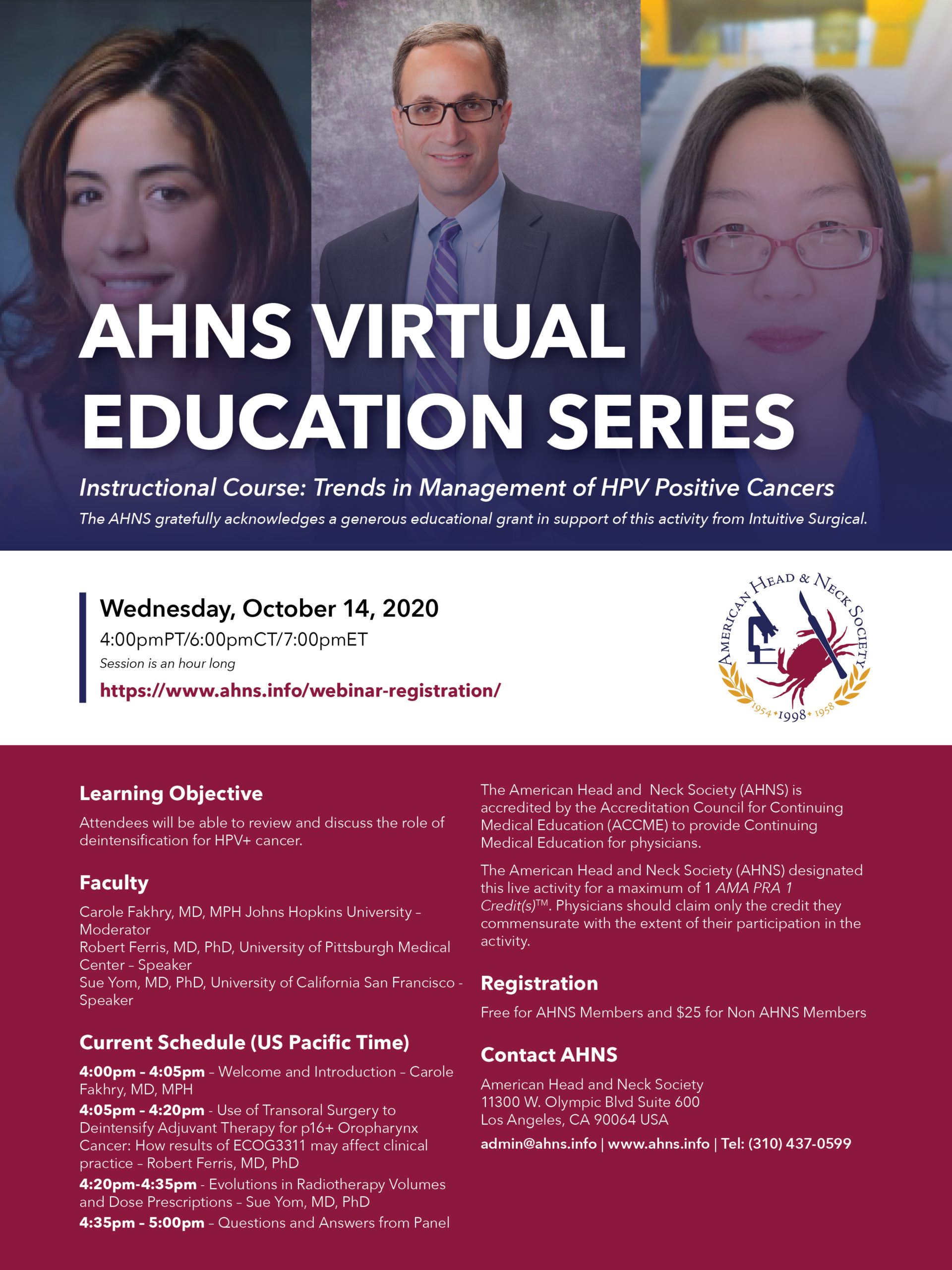
AHNS Virtual Education Series
Trends in Management of HPV Positive Cancers Instructional Course: Trends in Management of HPV Positive Cancers The AHNS gratefully acknowledges a generous educational grant of this activity from Intuitive Surgical. Date: Wednesday, October 14, 2020 Time: 4:00 PM Pacific /6:00 PM Central / 7:00 PM Eastern Session is an hour long Register Here Learning Objective: …