Artificial Intelligence in Management of H&N Cancer: New Horizons Presented
Artificial Intelligence in Management of H&N Cancer: New Horizons Presented by the AHNS Population Health & Clinical Research Service #AHNS #AHNS2025 #COSM2025 #AI #H&N
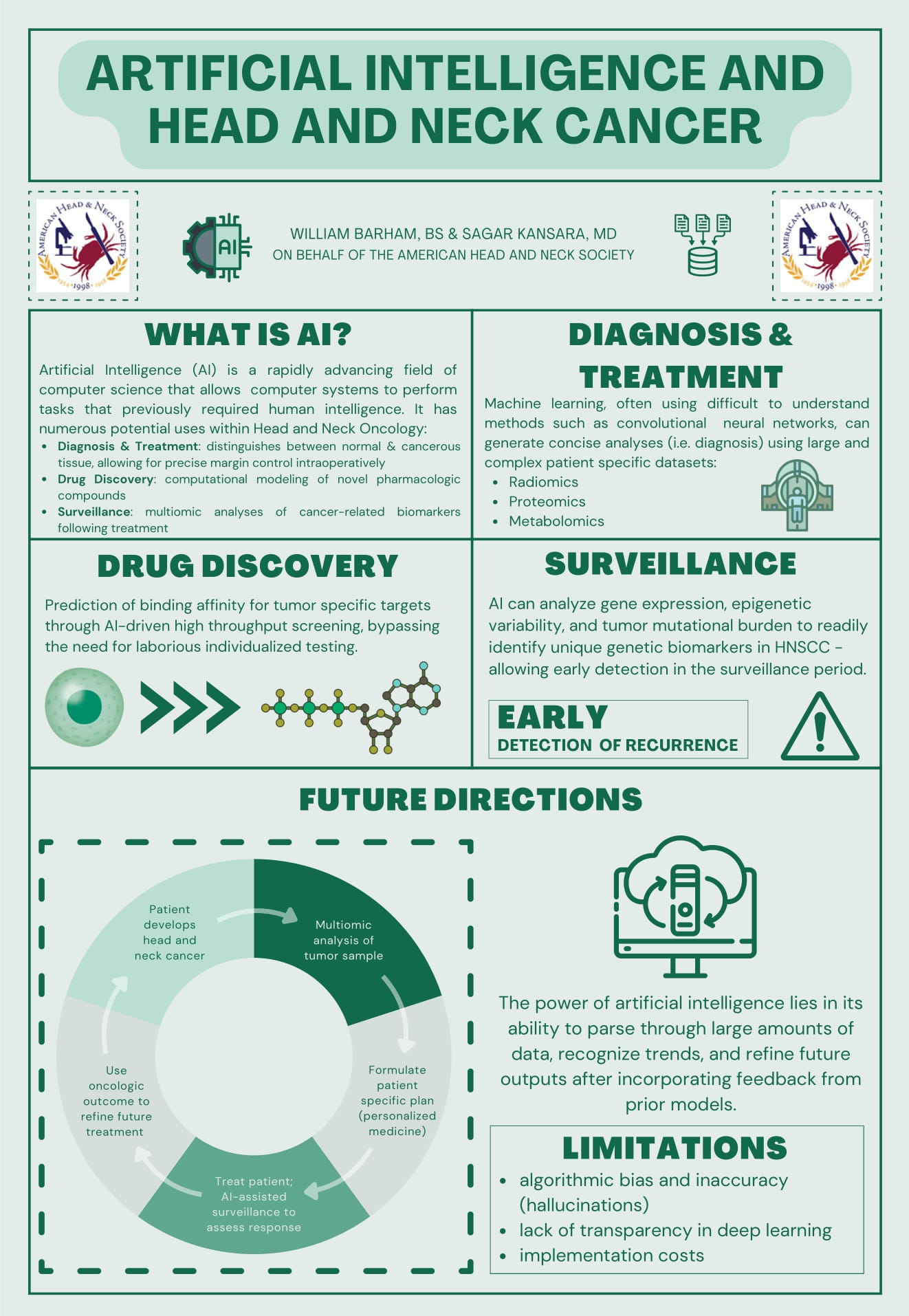
Artificial Intelligence in Management of H&N Cancer: New Horizons Presented by the AHNS Population Health & Clinical Research Service #AHNS #AHNS2025 #COSM2025 #AI #H&N

A conversation with Ravindra Uppaluri, MD, PhD “Neoadjuvant Therapy for Advanced H&N Mucosal Carcinoma” with Sagar Kansara, MD Presented by the AHNS Population & Health Clinical Research Service Watch Now!

The end of April Head and Neck Cancer Awareness month approaches, please spread awareness about Oral Cancer where early detection will save lives and improve outcomes! Signs and symptoms that should prompt medical attention include 1. Growing bump in the mouth 2. Persistent sores or white or red patches 3. Persistent pain or difficulty speaking …
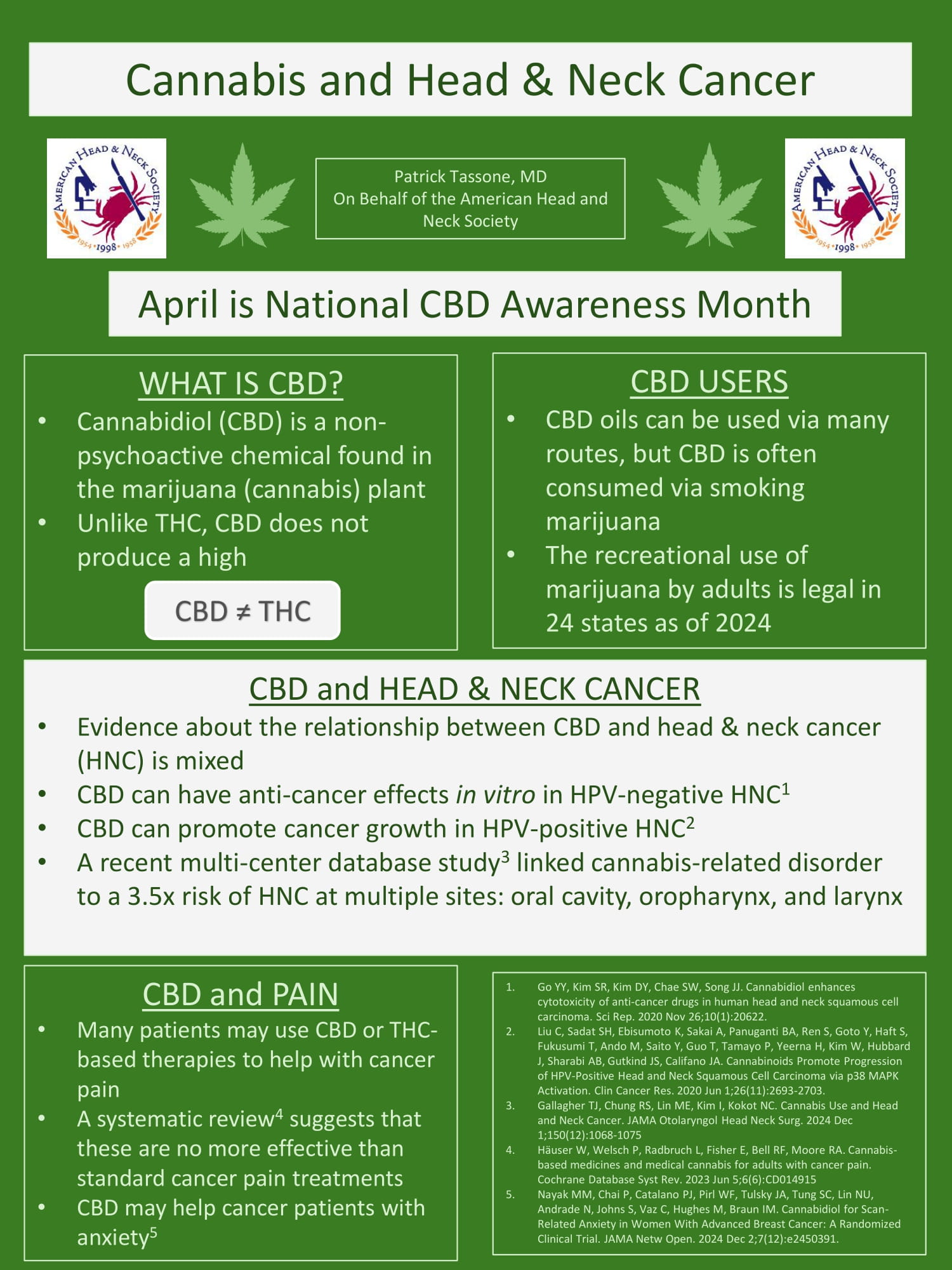
April is National CBD Awareness Month! Many patients with head & neck cancer have questions about the evidence regarding the use of cannabis and cannabidiol. This infographic offers facts about cannabis, CBD, and head & neck cancer.
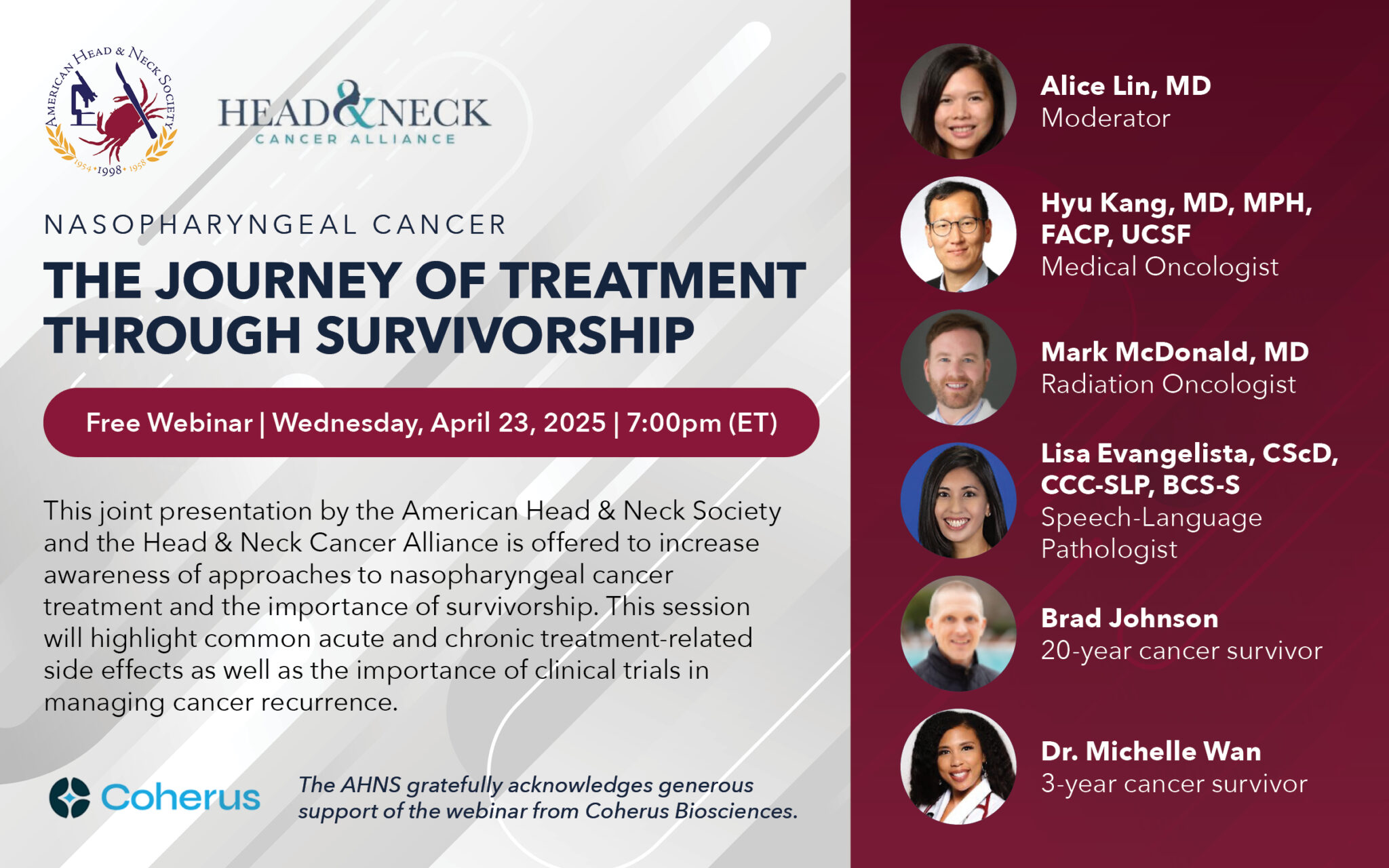
The AHNS gratefully acknowledges generous support of the webinar from Coherus BioSciences Wednesday, April 23, 2025 – 7:00 PM Eastern Time This Joint presentation by the American Head & Neck Society and the Head & Neck Cancer Alliance is offered to increase awareness of approaches to nasopharyngeal cancer treatment and the importance of survivorship. This …
